THE THYROID IN PREGNANCY
Pregnancy is an extremely novel experience, with many biological and biochemical changes happening within. It is said that pregnancy is a ‘stress test’ for the body’s systems. This is especially so for the thyroid. Pregnancy has a profound impact on the thyroid gland and its function. A mother’s thyroid function will increase by up to 50% to accommodate for the physiological changes in pregnancy. Let’s explore this impact, understand why thyroid monitoring is important during pregnancy, and better understand increased iodine requirements. First up, if you haven’t read my previous blog on the thyroid basics, you can start there.
Thyroid Hormone RoleS
During pregnancy, optimal thyroid function is essential for the growth and development of the baby, regulating brain and nervous system development (neuronal migration, connection, myelination and synaptogenesis). In this way, thyroid hormones are crucial for brain maturation, impacting IQ, and neurodevelopment. Thyroid dysfunction in pregnancy can also negatively impact obstetric outcomes and general foetal wellbeing.
THE NEED FOR MORE THYROID HORMONES
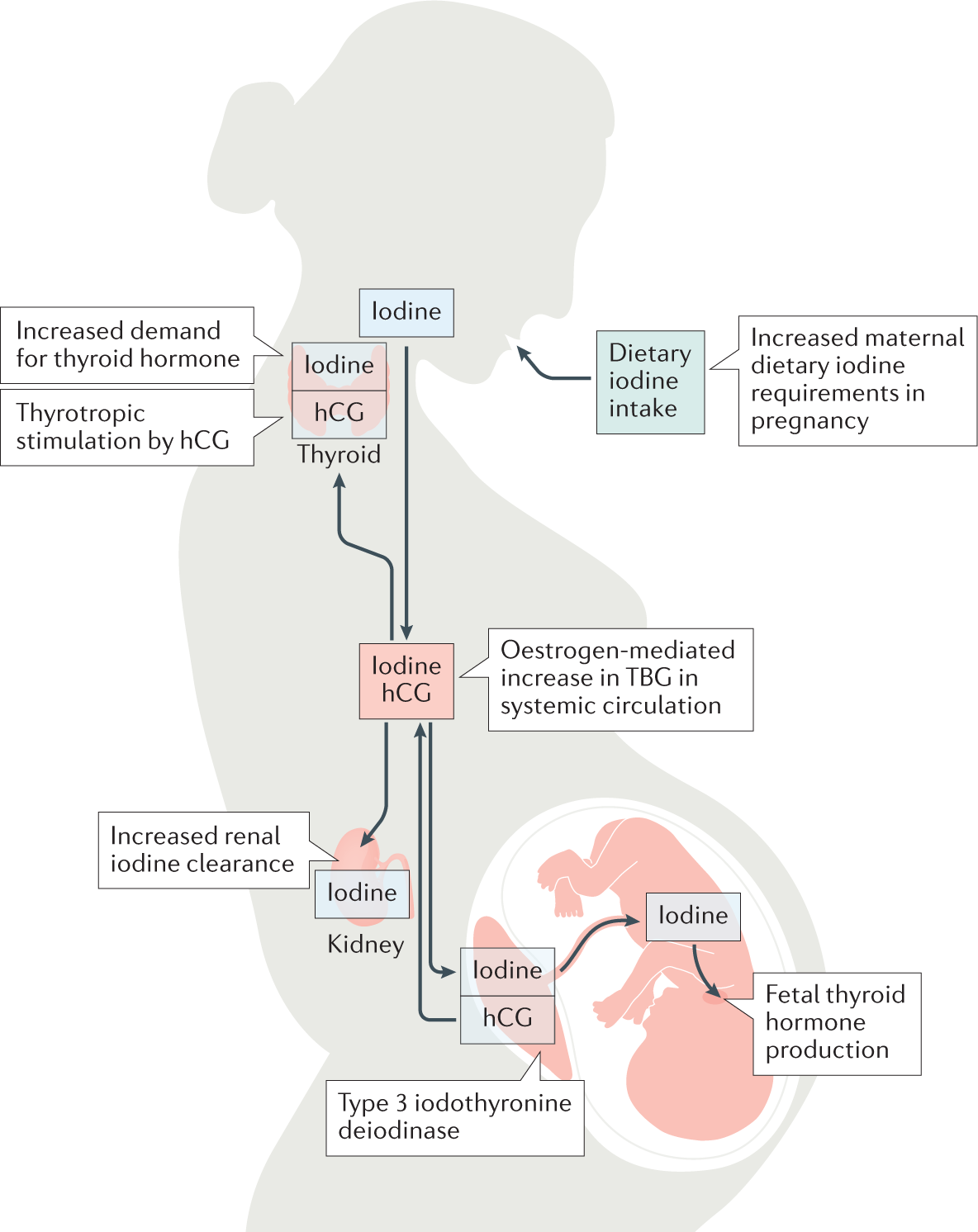
Bub’s Thyroid Hormone Needs: Up until about midway through the second trimester, a baby’s thyroid is entirely dependent on the mother’s thyroid hormones until its own thyroid takes over. At 10-12 weeks gestation, bub’s thyroid will begin to concentrate iodine, but not until around week 20 will its thyroid start to synthesise and secrete thyroid stimulating hormone (TSH) to create its own hormones. Therefore, a mother’s thyroid has to work harder to provide thyroid hormones for both bub, and herself.
hCG acts on the TSH Receptor: Shortly after conception, placental human chorionic gonadotropin (hCG) levels directly stimulate the TSH receptor, increasing production of thyroxine (T4). Negative feedback then causes a decrease in TSH. In trimester one, the largest drop in TSH will be observed, with a gradual rise in the second and third trimesters. Please note: The downward shift in TSH will be greater in multiple pregnancies (twins) than in singleton pregnancies.
Increased thyroid enzymes: The enzyme 3 iodothyronine deiodinase is responsible for the degradation of T4 and triiodothyronine (T3), which is expressed in abundance in the placenta, chorion, and amnion. This increases rT3 in pregnancy. This could be a protective effect due to the increased metabolic demands in pregnancy and to keep the foetus safe. T3 being deemed ‘too scary’ in pregnancy.
Oestrogen-mediated Increase in TBG: Increased levels of oestrogen in pregnancy causes a twofold rise in thyroxine-binding globulin (TBG). This decreases the bioavailability of thyroid hormones as more are bound to transporter proteins. This increases the need for greater thyroid hormone production, as less are bioavailable.
Increased Plasma Dilutes Thyroid Hormones: Increasing plasma levels in pregnancy mean thyroid levels are also diluted.
Iodine REQUIREMENTS
Iodine requirements increase by 50% in pregnancy. Because of this, the thyroid gland grows by 10% in iodine replete women and can grow from 20-40% in iodine depleted women. The thyroid works to ‘trap’ iodine like a venus fly trap to use it to make thyroid hormones. Increased needs are because of all that has been outlined above: The need to directly supply bub with T4, increased degradation, increased metabolic demands, and the oestrogen mediated increase in TBG. Additionally, loss of iodine occurs from increased renal excretion. The minimum requirement of iodine is 150 µg daily, with the recommended dose between 220-250µg daily during pregnancy. It is ideal to have replete iodine levels before conception, however, addressing levels as soon as is reasonably possible is advised. Urinary iodine is a great test to do to better understand levels. This can be completed in the preconception phase before starting any prenatal vitamins and/or during pregnancy whilst supplementing with iodine to see your status (and that the supplementation you are on is adequate).
Please note: In hyperthyroidism, Graves’ disease, or the presence of thyroglobulin antibodies, iodine intake must be monitored and potentially avoided. Please seek individualised assessment before commencing any supplement regime. Too much iodine is not a good thing!
IN SUMMARY
There are many physiological changes in pregnancy, and many that impact the need for additional thyroid hormones. This increases iodine requirements. Pregnancy is like a ‘stress test’ for the thyroid and so monitoring thyroid levels is wise. Stay tuned for the next blog in the thyroid series where we address thyroid management when something goes astray, or in already existing thyroid disease. Please remember to seek qualified practitioner assistance when starting any new supplement regime. Over supplementing with iodine can be dangerous, especially in conditions that can be aggravated by iodine (i.e. Graves, hyperthyroidism, and presence of TgAb).