EVERYTHING WE NEED TO KNOW ABOUT OVULATION
The mechanics of a menstrual cycle are commonly misunderstood. A misconception that I myself actually had before studying naturopathy was that if I had a menstrual bleed, it meant that I had ovulated. A patient brought this same belief up in clinic last week and then I asked my followers on Instagram the question. Out of over 100 people, 11% thought that having a menstrual bleed meant ovulation occurred, 26% were not sure, and 63% realised that a menstrual bleed did not always mean ovulation occurred. Of course, I am sure some of these were guesses, but enough people are unsure or believe menstrual bleeds equal ovulation that it prompted me to explain anovulatory cycles. Herein, I am busting the myth that if you have had a menstrual bleed you have definitely ovulated. Now let me explain…
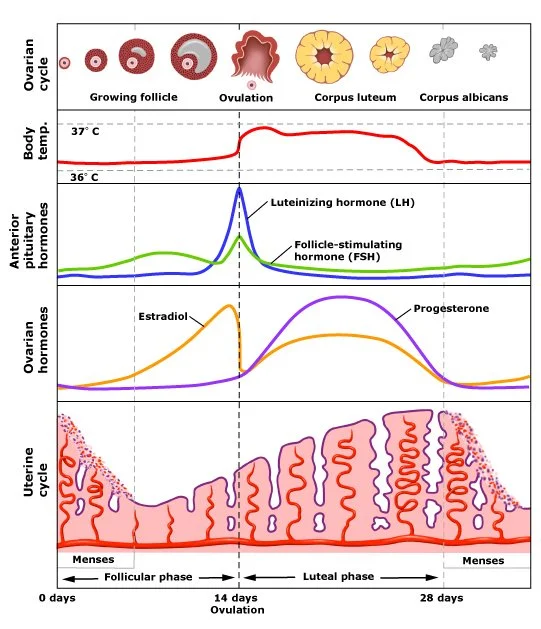
In a normal menstrual cycle, the brain communicates with the ovaries with two hormones (Follicle Stimulating Hormone; FSH, and Luteinizing Hormone; LH). Their job is to develop the chosen ovarian follicle for the month to the point that it is ready to ovulate the egg, or oocyte, which is inside the follicle (inside the ovary). Stimulation of FSH and LH as prompted by the brain causes the release of oestrogen from the ovary, which is important for beginning the development of the uterine lining after menses, as well as peaking mid-cycle, alongside an LH-surge, to establish ovulation. This process is a beautifully coordinated orchestra.
Once ovulation has occurred, the follicle that housed the egg now becomes the corpus luteum and releases our lovely luteal hormone progesterone. This balances out the luteal phase rise in oestrogen. As oestrogen continues to proliferate our lining of the uterus, progesterone prepares the womb to receive and nourish the embryo (fertilised egg) if implantation occurs. When it doesn't, negative feedback lets the brain know conception hasn’t happened, menstruation occurs, and the cycle begins again.
The thing is, this is not always the way things go. Many factors interfere with ovulation, or the intricate dance of hormones required for ovulation to occur. These include stress, undereating, eating disorders, overtraining, being underweight, infections, irregular circadian rhythm, disordered thyroid function, medications, polycystic ovarian syndrome (PCOS), and of course low antral follicle count. The hypothalamic-pituitary-ovarian axis, or the hormonal highway between brain and ovary, can be impacted acutely (say if there was an intensely stressful occurrence one month), or chronically (continued period without ovulation occurring). Because a one-off missed ovulation is nothing to be concerned about and is a normal protective response of the body—the brain thinks: If you conceived during this stressful period, it could be a disaster. Our body is intelligent. So, what about when it’s happening over and over?
Anovulatory cycles can be regular (26-32 days), though oftentimes will be irregular. Having a cycle really often (i.e. every 14 days), or it is blowing out for months at a time, are signs that ovulation is not occurring. Please note that extended cycles can also mean it has taken a long time to ovulate, so long cycles do not always mean ovulation has not occurred. I know, I know, the female sex hormone orchestra is confusing!
Many women might be tricked into thinking ovulation occurred as they will still experience premenstrual symptoms (PMS) before a bleed where they didn’t ovulate. This is more so from the continual exposure to oestrogen without the lovely buffering effect of progesterone. This can mean periods are very heavy because of the continued proliferation of the uterine lining, there can be extreme breast tenderness, fluid retention, headaches, mood swings etc. But, PMS also doesn’t mean we have ovulated.
It also pays to mention that anovulatory cycles happen on hormonal birth control. The oral contraceptive pill (OCP) literally switches off your ovaries, with no stimulation from the brain to develop follicles to ovulation. Each ‘bleed’ that takes place on the OCP is a breakthrough bleed, not a ‘real’ period. The Mirena and copper IUD work differently, so ovulation can occur.
Okay, so let’s talk about signs of ovulation, so we can pinpoint what’s going on for us. First up, let me dispel another myth that cycle-tracking apps can tell us when we ovulate. Perhaps it does align with your ovulation, because your cycle is regular and considered normal against the population. However, there is no way a cycle tracking app can precisely determine ovulation. So please don’t rely on this. Ways we can discern if we have ovulated or not are from the presence of cervical mucus, a basal body temperature (BBT) rise, an LH surge (ovulation test), and/or a post ovulation blood test that shows the presence of progesterone.
Cervical mucus
In the lead up to ovulation, our cervix releases mucus that resembles egg white. This is like a slippery slide through the vaginal canal for sperm swimming toward the egg. Oestrogen rising toward ovulation plays a role in the mucus changes experienced. Once ovulation occurs, there is an abrupt discontinuation of egg-white type mucus from the rise in progesterone. So, the last day of cervical mucus (usually also the day of the most cervical mucus), is very likely ovulation.
Basal body temperature tracking
As you can see against the interplay of hormonal changes in the picture below, there is also a change in temperature that happens after ovulation. Progesterone causes this rise in BBT, so we know if our temperature increases (for at least 3 days in a row), we have ovulated.
LH surge/ovulation test kit
There are ovulation test kits we can use to understand when the LH-surge occurs, which corresponds with ovulation. However, we can have an LH surge without ovulation occurring, so I wouldn’t rely on this alone to determine ovulation is definitely happening.
7-days post ovulation (7DPO) blood test
Blood testing in the luteal phase can show whether progesterone is present or not. Good practice is doing this test 7 days post ovulation. This can be determined by any of the above measures. Testing oestrogen and progesterone at this time can tell us not just about ovulation, but also about the luteal phase in general. This is important for understanding menstrual disturbance such as luteal phase defect, PMS issues, heavy and/or painful periods, infertility and more. Ideally, if we see progesterone ≥5 nmol/L then ovulation has occurred.
In essence, the menstrual cycle is a vital sign. It tells us so much about our overall health, with any disruptions presenting little whispers of how we can reestablish balance. Ovulatory cycles are also banking health for later. Every ovulation and exposure to the dance of hormones that move through us is clocking up health for our postmenopausal years when our exposure to these hormones declines. Ovulatory cycles promote brain, bone and cardiovascular health in our later years. Every ovulation adds to that, and every missed ovulation is a missed opportunity at preventing age-related diseases such as osteoporosis, Alzheimer’s and metabolic disease. A big reason to sit with whether hormonal birth control is actually right for you (a discussion for another day, perhaps!).
I created RHYTHM, a free online course, that explains the biology if our menstrual cycle in-depth, teaches basal body temperature tacking, and also moves through the inner seasons of our cycle so we can understand changes in energy, mood and motivation better (with many supports and focuses to help us align to where we are at cyclically). To access it, you can do so here. It goes into a bit more depth of what we have spoken about today.
If you feel you would benefit from a menstrual cycle tune-up, you are most welcome to book an appointment to see me in clinic. Any one of the lovely naturopaths at Perth Health and Fertility also specialise in this area and so there are many options for you to explore your menstrual health with someone most suited and optimise this intricate and beautiful vital sign.